What is it about?
Antimicrobial resistance (AMR) is an increasing threat to global health. AMR is a leading cause of death around the world, with the highest burdens in low-resource settings. The risks and sanitary consequences of AMR are disproportionately experienced by those living in Low- and Middle-Income Countries (LMICs). While addressing antibiotic use has largely been documented in hospital settings, the understanding of social drivers affecting antibiotic prescribing and dispensing practices in the context of human and animal health in primary care (PC) in LMICs remains extremely limited.
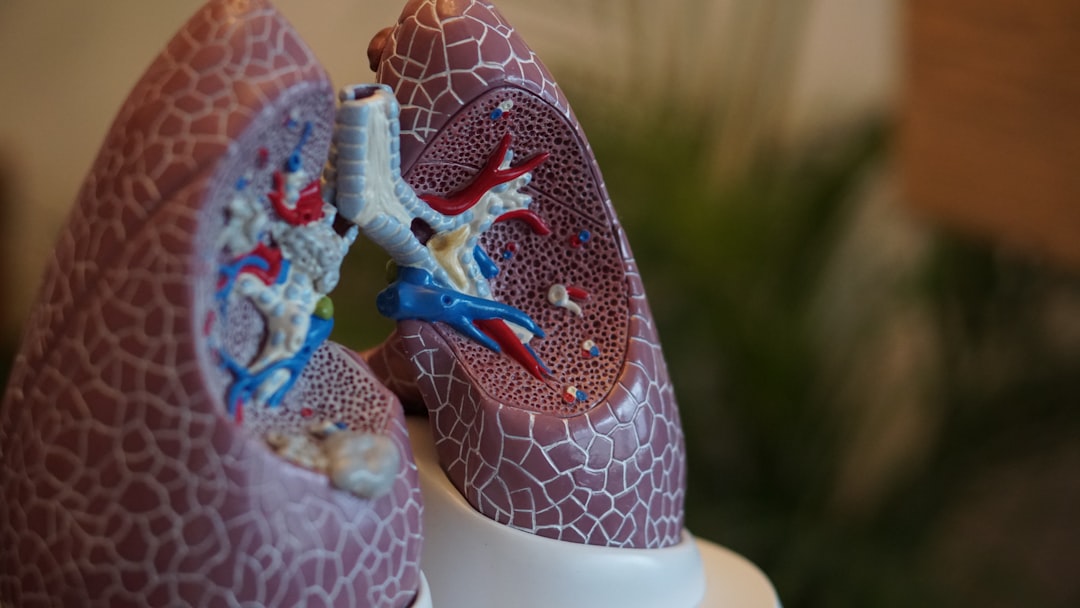
Featured Image

Photo by Aditya Romansa on Unsplash
Why is it important?
Our study aimed to explore the social drivers related to inappropriate prescriptions of AB, presenting results of the social implications of this increasing public health threat in the context of PC of human and animal health in Brazil. Through a relational One Health perspective between social drivers affecting AMR and PC we identified that in-locus factors influencing antibiotic prescriptions and dispensing practices are intertwined with individual accounts of risk management, systemic contradictions and ambivalences in the national health system. In other words, HPs experience contextual and territorial challenges that directly influence their risk perception, diagnosis, use of laboratorial and image exams, time and decision to undergo treatment, choice of AB and strategies in coping with AB prescriptions. Our findings suggest interventions tackling AB use and AMR in Brazil should consider the social context, the complex health system structure and current integrated programs and services in PC.
Perspectives
I our view, qualitative studies offer not only pathways for further examination extrapolating certain contexts, but they also reveal the pervasiveness of distal and structural social relations affecting microlevel activities. This approach allowed us to reflect on the complexities involving socially deprived populations, the social production of risks and the challenges health systems face in responding to the increasing global threat of AMR. Political actions are needed to tackling these problems at the level of PC through local-sentive and long-term health care interventions.
Roberto Brandao
Universidade de Sao Paulo Campus da Capital
Read the Original
This page is a summary of: Coping with in-locus factors and systemic contradictions affecting antibiotic prescription and dispensing practices in primary care–A qualitative One Health study in Brazil, PLoS ONE, January 2023, PLOS,
DOI: 10.1371/journal.pone.0280575.
You can read the full text:
Contributors
The following have contributed to this page