What is it about?
Health information technology (HIT) is an area of computer technology concerned with the design and development of systems to generate and store healthcare-related information and make use of that information. Healthcare organisations that use HIT, for instance, such as an ePrescribing system, are expected to have lower costs, improved efficiency and reduced errors while also giving better services and patient care. In order to know if HIT systems are really as good as might be expected, we need methods to study the effects – or end-points - of using HIT systems in healthcare organisations. Here, the authors seek to develop a protocol for evaluating the cost-effectiveness of ePrescribing systems in four hospitals in the UK. In two of the hospitals, ePrescribing systems are to include extensive clinical decision support (CDS). In addition to ordering medications, systems with CDS offer health professionals advice and onscreen alerts to aid decision making while they are prescribing. In the other two hospitals, the ePrescribing systems are more basic systems. The method the authors describe for evaluating the ePrescribing systems is a statistical method called Bayesian probability logic. This is a type of statistics that uses knowledge of prior events to help to predict future events. For a cost-effectiveness evaluation of ePrescribing systems, we need to consider the costs and the benefits of limiting the number of adverse drug events (ADEs). To do that requires identifying adverse events, the expected health benefits, the cost of the HIT system, and the cost consequences of avoided adverse events. No single event can totally capture the effectiveness of an ePrescribing system, and these authors describe observing changes in error rates and adverse events in four error categories (that is, of errors resulting in: death; permanent disability; moderate disability; and minimal effect). The authors suggest using both quantitative and qualitative data from different sources in order to find evidence for or against the cost-effectiveness of ePrescribing systems. This protocol is designed to help address the criticism that evaluations of HIT systems do not capture all the relevant end-points. The authors argue that evaluations of ePrescribing systems cannot ignore multiple end-points merely because they are difficult to observe and to analyse. This protocol seeks to include as many variables as possible in the cost-effectiveness analysis. The authors conclude that there is still room to better understand the full impact of ePrescribing systems on preventing adverse events in hospitals. The protocol they describe offers a method for evaluating the cost-effectiveness of ePrescribing systems, which could also be useful for evaluating other HIT systems.
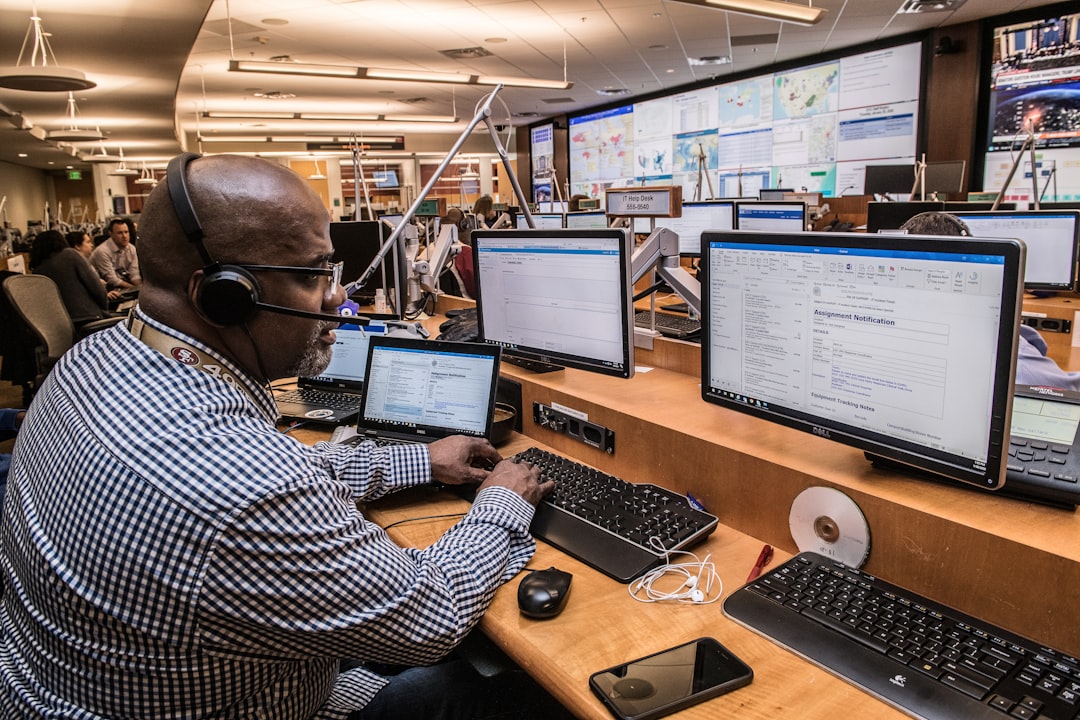
Featured Image
Read the Original
This page is a summary of: Protocol for evaluation of the cost-effectiveness of ePrescribing systems and candidate prototype for other related health information technologies, BMC Health Services Research, July 2014, Springer Science + Business Media,
DOI: 10.1186/1472-6963-14-314.
You can read the full text:
Contributors
The following have contributed to this page