What is it about?
After aneurysmal subarachnoid hemorrhage (SAH), both proximal and distal cerebral vasospasm can contribute to the development of delayed cerebral ischemia. Intra-arterial (IA) vasodilators are a mainstay of treatment for distal arterial vasospasm, however there are no well-established methods to assess the efficacy of interventions in real-time. This study validates an algorithm for continuous assessment of distal cerebral arterial changes in response to IA vasodilator infusion in patients with vasospasm and aneurysmal SAH, which has the potential for clinical use in the future.
Featured Image
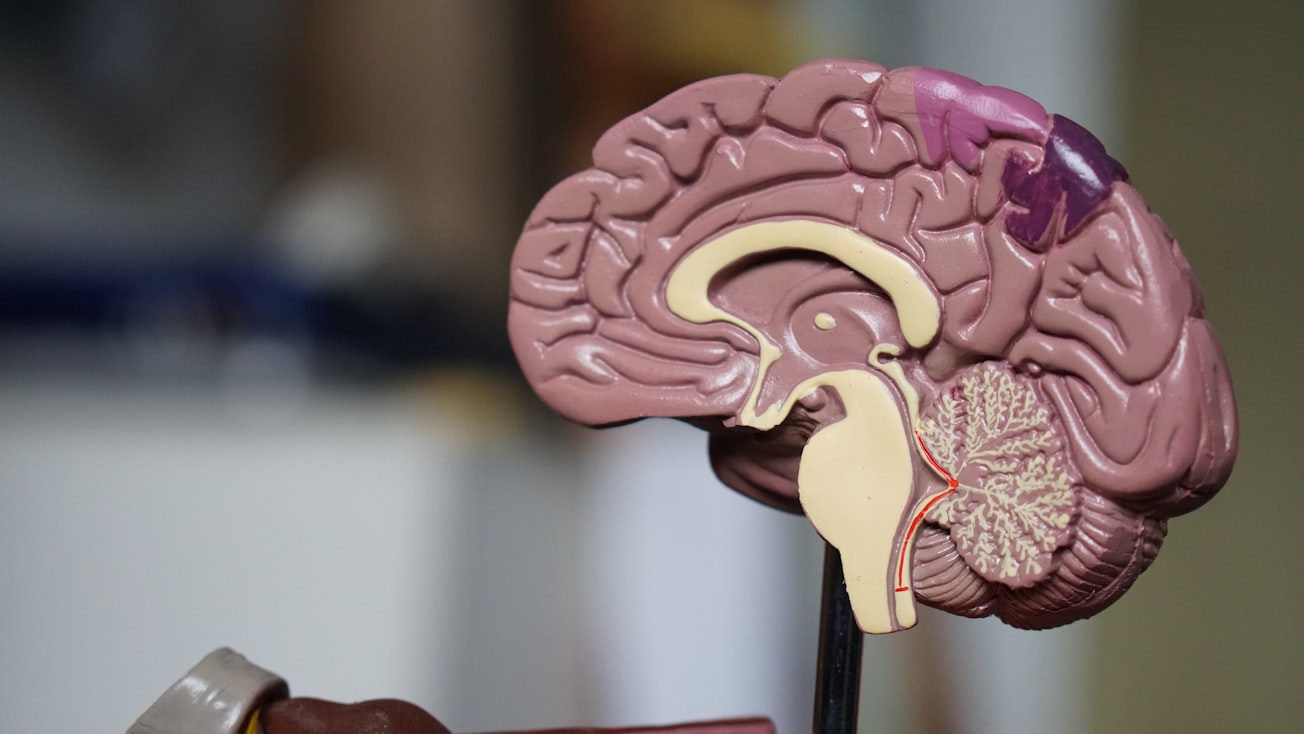
Photo by Robina Weermeijer on Unsplash
Why is it important?
The premise of our approach is that distal cerebral arterial changes induce a consistent pattern in the morphological changes of intracranial pressure (ICP) pulse. This premise was demonstrated using a published algorithm in previous papers. We applied the algorithm to calculate the likelihood of cerebral vasodilation (VDI) and cerebral vasoconstriction (VCI) from intra-procedural ICP signals that are synchronized with injection of IA vasodilator verapamil. The result showed that the VCI was significantly lower after the first verapamil injection than VCI at baseline. Larger dosage of verapamil injection results in larger and longer VDI increase.
Perspectives
We hope this article provides clinicians a potential method for continuous assessment of distal cerebral arterial changes in response to IA vasodilator infusion in patients with vasospasm and aneurysmal SAH.
Xiuyun Liu
Johns Hopkins University
Read the Original
This page is a summary of: Morphological changes of intracranial pressure quantifies vasodilatory effect of verapamil to treat cerebral vasospasm, Journal of NeuroInterventional Surgery, January 2020, BMJ,
DOI: 10.1136/neurintsurg-2019-015499.
You can read the full text:
Contributors
The following have contributed to this page







