What is it about?
Antipsychotics exert their antipsychotic effects by blocking dopamine D2 receptors. The D2 receptors targeted for antipsychotic action are those in the mesolimbic system. D2 receptors are also expressed in the pituitary gland and inhibitively regulate prolactin. The vast majority of antipsychotics do not have the ability to selectively act on specific sites. Therefore, antipsychotics block the D2 receptors in the pituitary gland, which releases the inhibition of prolactin secretion and increases prolactin secretion. Only one antipsychotic, aripiprazole, a partial agonist of D2 receptors, stimulates prolactin secretion to a certain extent, but all other antipsychotics stimulate prolactin secretion and induce hyperprolactinemia. Hyperprolactinemia is a frequent and serious adverse effect of antipsychotic medication. Antipsychotic-induced hyperprolactinaemia occurs overall in up to 70% of patients with schizophrenia, depending on the medications used. Hyperprolactinemia may cause sexual dysfunction, amenorrhea, infertility, galactorrhea, and osteoporosis, which in general relates to the degree of prolactin elevation. Hyperprolactinemia is particularly likely to cause health problems in female patients. A recent Finnish epidemiological study showed that patients taking prolactin-elevating antipsychotics for more than five years had a higher risk of breast cancer. Antipsychotic-induced hyperprolactinemia should not be left untreated.
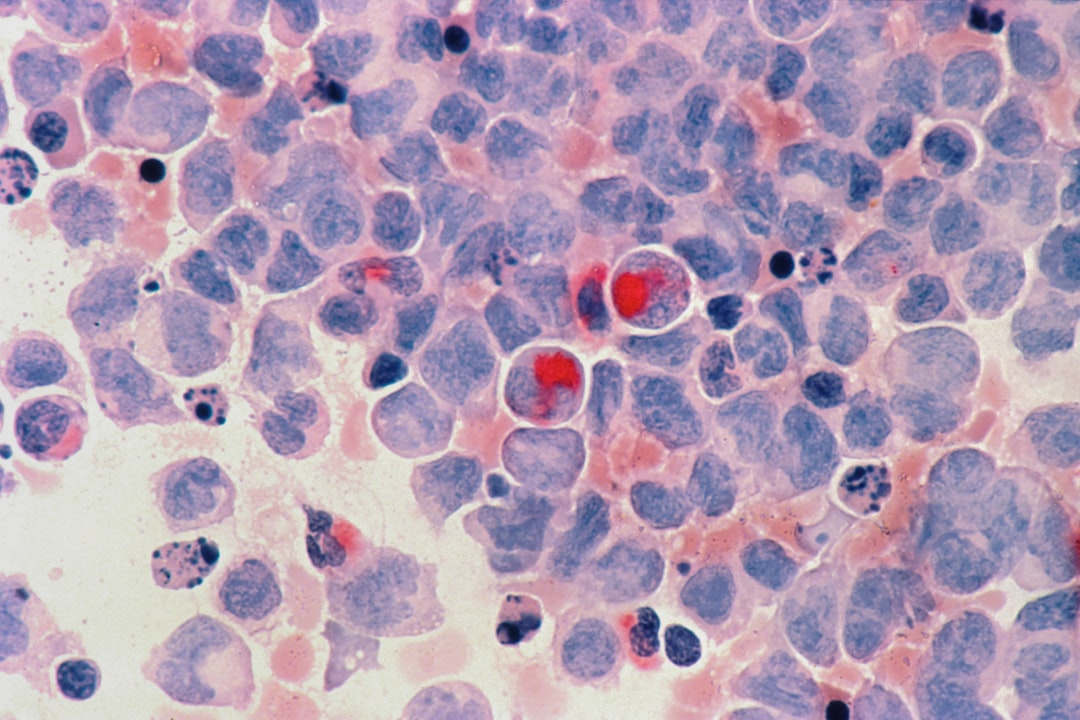
Featured Image

Photo by Victoria Strukovskaya on Unsplash
Why is it important?
When antipsychotic-induced hyperprolactinemia warrants treatment, several approaches can be attempted, such as dose reduction of the offending antipsychotic, switch to a prolactin-sparing antipsychotic (i.e. aripiprazole, olanzapine, quetiapine or clozapine), addition of a dopamine partial agonist (aripiprazole) to the current regimen, and addition of a dopamine agonist (i.e. bromocriptine or cabergoline). There is limited evidence for the management of antipsychotic-induced hyperprolactinemia, and these strategies, however, carry the risk of precipitating an exacerbation or relapse of psychotic symptoms, which may put the patient at a greater risk for adverse consequences, possibly worse than experiencing hyperprolactinemia itself. We are investigating the regulation of prolactin outside of the pituitary dopamine system, which is the main regulatory circuit for prolactin. This is the GABAergic nervous system of the pituitary gland, an inhibitory nervous system. The GABAergic nervous system of the pituitary gland inhibits the dopaminergic nervous system, which cancels the inhibition of prolactin secretion by dopamine, so prolactin secretion occurs. However, if the pituitary dopaminergic system has already been blocked by antipsychotic drugs, this mechanism will not work. Furthermore, when prolactin-secreting cells increase prolactin secretion, GABA receptors are expressed on them and inhibit prolactin secretion. Therefore, in patients with hyperprolactinemia caused by antipsychotic drugs, administration of GABA to the pituitary gland may inhibit the distribution of prolactin. There are many ways to increase GABA, but we thought of administering L-carnitine as a way to increase GABA without affecting other functions. Carnitine is used for GABA biosynthesis in the brain. Levocarnitine was coadministrated over a period of three months in seventeen psychiatric inpatients treated with antipsychotics and valproate. As serum carnitine levels increased from 64.2±4.5μmol/L to 94.2±6.4μmol/L, the prolactin levels decreased from 59.0±9.4ng/ml to 42.1±11.3ng/ml. The ratio of prolactin levels at one month against baseline was significantly negatively correlated with the ratio of acylcarnitine/free carnitine levels at one month against baseline. Carnitine attenuates antipsychotic-induced hyperprolactinemia in a concentration-dependent manner. Proactin lowering effect of GABA is a receptor-mediated event, where the high affinity receptor population is present. Scince antipsychotic-induced hyperprolactinemia may induce high affinity receptors like suckling, GABA reduces prolactin levels through pituitary GABA receptors.
Perspectives
Although the main physiological control of prolactin secretion is exerted by the inhibiting action of dopamine, anterior pituitary GABA receptors have been shown to play a functional role in the inhibitory control of prolactin secretion. Carnitie attenuates antipsychotic-induced hyperprolactinemia by stimulating pituitary GABA receptors. This mechanism is irrelevant to the dopaminergic system, therefore psychotic symptoms may not be aggravated. If hyperprolactinemia caused by antipsychotic drugs is left untreated, there is a risk of various health problems. Large-scale, long-term studies need to be conducted to determine whether concomitant administration of carnitine is effective in reducing breast cancer and bone fractures. There are also gender differences in the metabolism of antipsychotics, with women tending to have higher concentrations. Since high prolactin tends to increase the risk of femoral neck fracture and breast cancer in women, it is important to conduct this study with gender differences in mind.
Takahiko Nagamine
Sunlight Brain Research Center
Read the Original
This page is a summary of: Pituitary gamma-aminobutyric acid receptor stimulation by carnitine may be a new strategy for antipsychotic-induced hyperprolactinemia, Psychiatry and Clinical Neurosciences, July 2017, Wiley,
DOI: 10.1111/pcn.12542.
You can read the full text:
Contributors
The following have contributed to this page