What is it about?
This study evaluated the demographic profiles and prevalence of serologic markers among donors who used CUE. We analyzed 2 years of donation data and 10 years of CUE records to assess the effectiveness of CUE and guide public policies regarding use of CUE for enhancing blood safety without seriously jeopardizing the blood supply by dropping CUE.
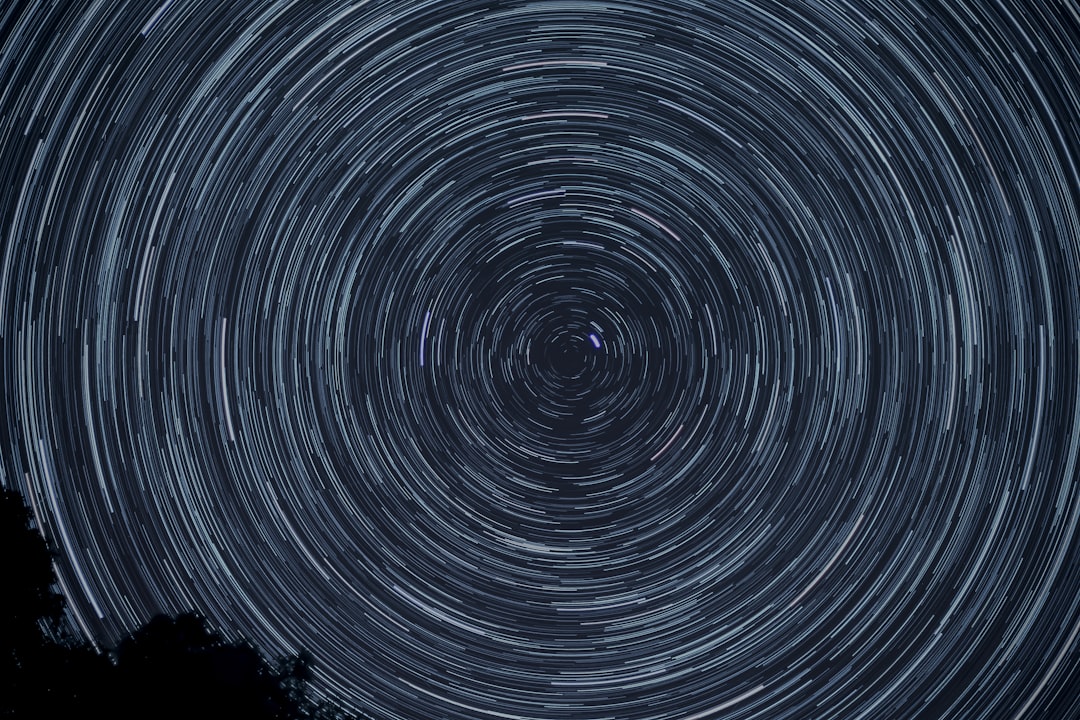
Featured Image
Why is it important?
The number of units discarded due to CUE has increased progressively over the years and the CUE‐related discard rate will increase even more considering the target of enhanced efforts to expand the repeat donor pool as a source of safe blood supply. In some countries CUE had minimal effectiveness in reducing transmission of infectious diseases by window period units.
Perspectives
Our results indicate that units from donors who used CUE at the current donation are more likely to have markers of transfusion‐transmitted infections than those units from donors who did not use CUE. However, when donors who used CUE in the past did not use CUE for a new donation, the infectious disease marker rates among these subsequent donations were the same as in donors who never used CUE. Therefore, we recommend that the procedure of discarding units because of CUE in the past should be discontinued.
Dr Cesar de Almeida-Neto
Faculty of Medicine, University of São Paulo
Read the Original
This page is a summary of: Demographic characteristics and prevalence of serologic markers among blood donors who use confidential unit exclusion (CUE) in São Paulo, Brazil: implications for modification of CUE polices in Brazil, Transfusion, January 2011, Wiley,
DOI: 10.1111/j.1537-2995.2010.02799.x.
You can read the full text:
Contributors
The following have contributed to this page