What is it about?
Hemochromatosis is a disorder of the iron metabolism, characterized by high body iron content, necessitating frequent phlebotomies to remove excess iron. In some countries, this blood is discarded and not used for blood transfusion because of the non-voluntary character of this donation, and because a potential risk of microbial contamination of the donor blood is assumed. A systematic review was performed in order to collect and critically examine solid evidence with regard to the effectiveness and safety of blood for transfusion when derived from hemochromatosis patients who do not suffer from complications or organ damage. Using three databases (The Cochrane Library, MEDLINE, and Embase) we searched for studies from date of inception until January 2012. Out of 3470 articles, 80 references that were relevant to our question were selected, including many opinion pieces, comments, letters, and narrative reviews. Based on our selection criteria, we finally retained only six observational studies, so evidence on this subject is scarce and furthermore, the strength of the available evidence is low to very low, due to poor study designs. We found no evidence that red blood cell concentrates from hemochromatosis patients without complications of iron overload do not comply with the physiological quality requirements for transfusion, nor that their blood would present a greater risk to recipient safety than blood from non-hemochromatosis donors. However, in vitro findings from two studies suggest that iron-overloaded patients would be more susceptible to bacterial growth, but future in vivo studies are warranted to confirm this. Based on this, we call for harmonization of the blood donor selection policy among countries allowing hemochromatosis patients who do not suffer from complications of iron overload to donate blood, once iron levels are normalized.
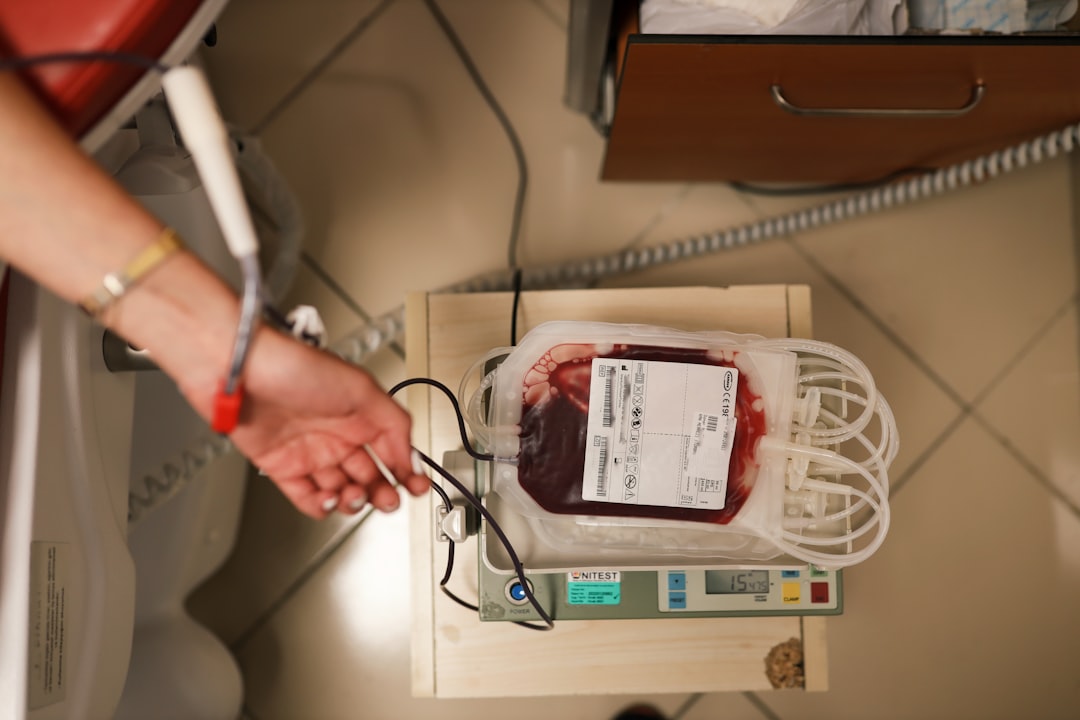
Featured Image
Read the Original
This page is a summary of: Is blood of uncomplicated hemochromatosis patients safe and effective for blood transfusion? A systematic review, Journal of Hepatology, November 2012, Elsevier,
DOI: 10.1016/j.jhep.2012.04.040.
You can read the full text:
Contributors
The following have contributed to this page