What is it about?
Numerous investigations into the opioid pandemic have shown that collaborative, conflict-free partnerships between patients and physicians help reduce inappropriate opioid prescribing. However, the requirements set by stricter policies make it necessary for doctors to begin conversations about overdose and addiction, which could potentially create tension with patients. This might put the cooperative relationships crucial for effective pain management at risk. The complex and controversial nature of opioid policies leads to the study of how physicians implement three recent policies at the time: (1) reguglar drug testing, (2) co-prescribing anti-overdose medication, and (3) transitioning patients from opioids toward alternative pain treatments. One strategy physicians used in implementing the 3 policies is pseudorequest—disguising mandates as suggestions, questions, or requests to frame decisions as if they are a product of collaboration. Examples of this strategy can be seen in phrases such as "my instruction for you today is that, maybe you have time to go upstairs to do some quick labs?" Another strategy physicians employ is audience broadening, whereby physicians justify their decisions as being the result of the patient's group membership so as not to come across as malicious, targeted, or isolated. Example phrases include "we're offering it (Naloxone) to all our patients that get, um, opioid prescriptions." The study also discuss in more detail the remaining face-saving acts used by physicians, whicch include downtoners, redirection, tag questions, impersonalization, listing, and (negative) imagery.
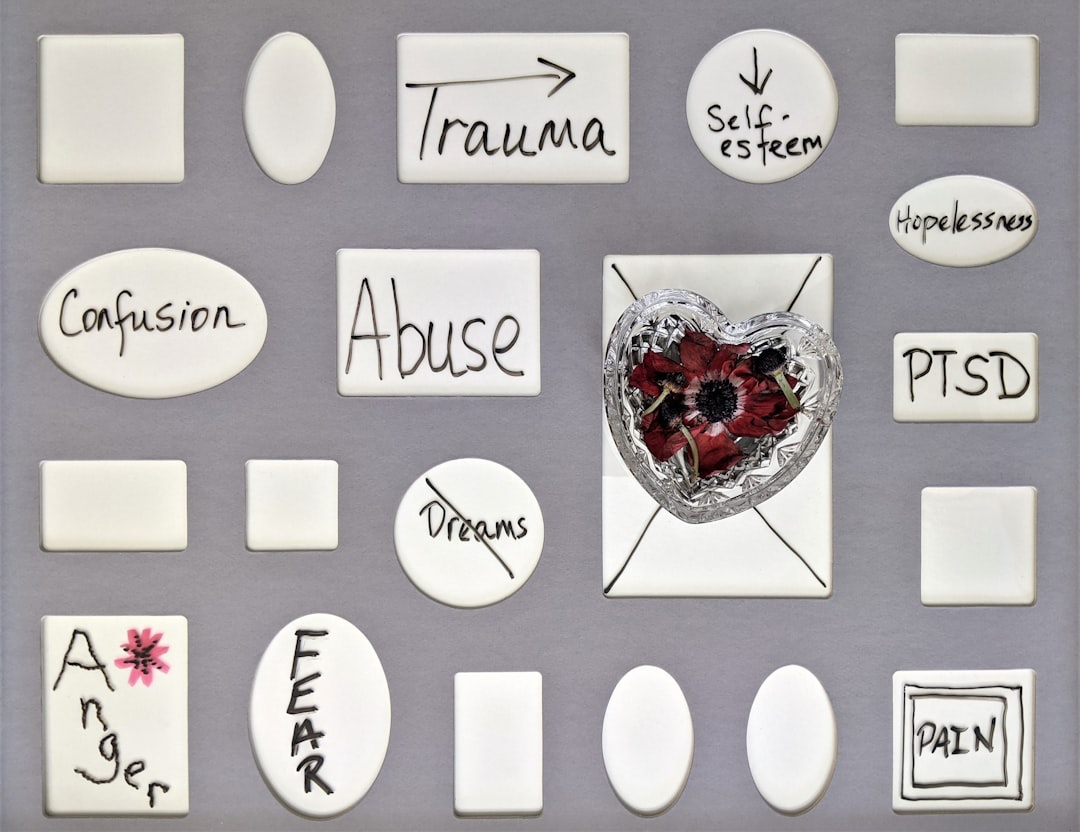
Featured Image

Photo by National Cancer Institute on Unsplash
Why is it important?
This study highlights the difficulties physicians face when implementing policies that limit patients' use of opioids. Many studies suggest that partnerships between doctors and patients are crucial in encouraging patients to explore alternative treatment options. However, the requirements set by stricter policies make it necessary for doctors to begin conversations about overdose and addiction, which could potentially create tension with patients. This study reveals that policymakers often fail to consider the communication challenges that physicians face due to their policies prioritizing the "What?" aspect while overlooking the "How?" aspect of putting them into action. This research suggests practical methods, such as creating rules requiring healthcare organizations to give doctors instructions on communicating policies to patients. This study emphasizes teamwork among healthcare organizations, doctors, and language experts in tackling communication difficulties between medical professionals and patients. By working together, they can enhance the effectiveness of pain management strategies.
Read the Original
This page is a summary of: Face-saving strategies and the burden of opioid policy enactments: When physicians’ compliance makes patients non-compliant, Journal of Pragmatics, February 2023, Elsevier,
DOI: 10.1016/j.pragma.2023.01.001.
You can read the full text:
Contributors
The following have contributed to this page