What is it about?
Alcohol use disorders, traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD) frequently coexist among US Veterans. In the current study we examined whether valproate was more effective than naltrexone (an active comparator) to prevent relapse into heavy drinking among a group of Veterans admitted to outpatient rehabilitation treatment. We did not find significant differences between the valproate and naltrexone group in the time to relapse to alcohol misuse. A history of moderate to severe TBI, however, was associated with poor treatment outcomes.
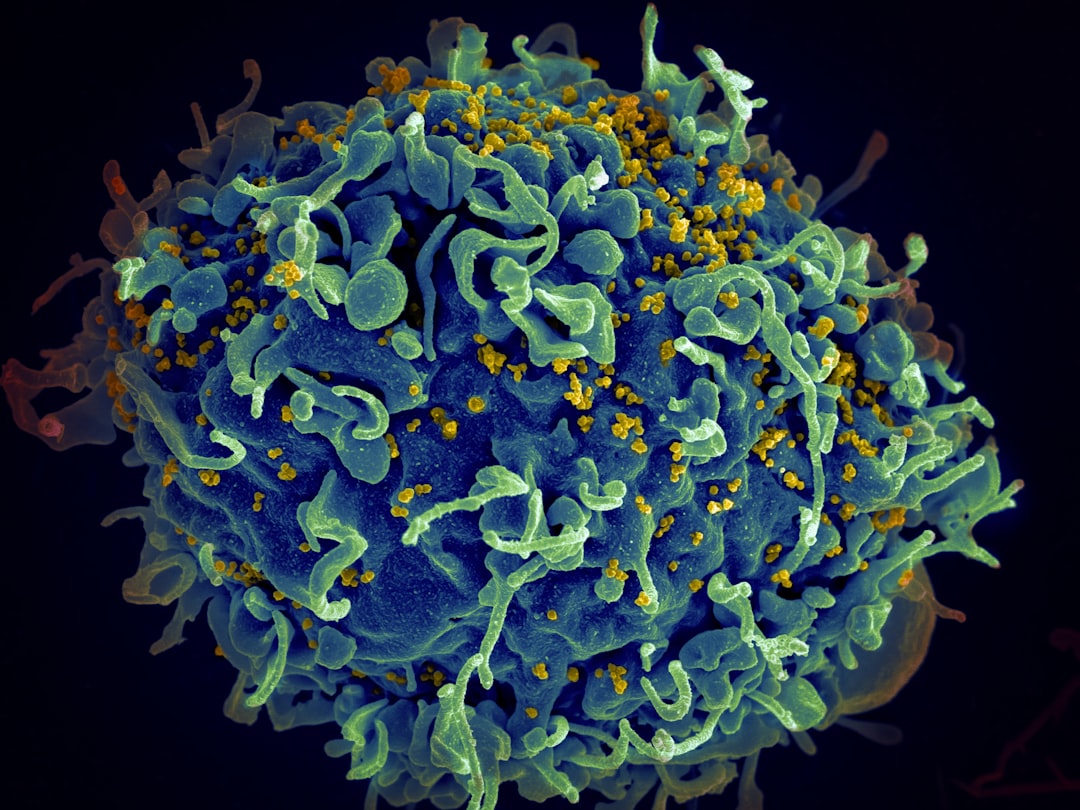
Featured Image
Why is it important?
Alcohol Use Disorders (AUD) are particularly frequent among US Veterans. They seldom occur in isolation and coexist with other conditions such as post-traumatic stress disorder (PTSD), mood and anxiety disorders and other forms of substance misuse (e.g. tobacco, cannabis and stimulant use disorders). In addition, a significant proportion of Veterans has a history of traumatic brain injury (TBI).There is a need to develop pharmacological options to treat AUD in this population. Furthermore, coexistent TBI and PTSD may influence treatment response and require a personalized treatment approach.
Perspectives
We will examine the structural and functional brain correlates that are associated with a poor outcomes following AUD treatment and clarify the etiologic contribution of TBI
Ricardo Jorge
Baylor College of Medicine
Read the Original
This page is a summary of: Treating Alcohol Use Disorder in U.S. Veterans: The Role of Traumatic Brain Injury, Journal of Neuropsychiatry, October 2019, American Psychiatric Association,
DOI: 10.1176/appi.neuropsych.18110250.
You can read the full text:
Contributors
The following have contributed to this page